Incontinence Advice
Overactive Bladders - What You Need To Know
Hundreds of thousands of people across the UK and Ireland suffer from an overactive bladder (OAB)1. If you suffer from an overactive bladder (OAB), you may experience urinary urgency, straining to pass urine, a strong and sudden urge to urinate (even if your bladder is empty), sudden incontinence of urine and often frequent urination throughout the day or night. An overactive bladder can impact your everyday activities, work schedule, and social interactions.
Here, we detail everything that you need to know about an overactive bladder.

What Is An Overactive Bladder?
Overactive bladder (OAB) is not a disease – it is the term used to refer to a particular group of urinary symptoms. Most people with an OAB experience frequent, sudden, and uncontrollable urges to go to the toilet, which can also be accompanied by leaking urine. Most people who struggle with these symptoms wake frequently in the night, or have a hard time falling asleep due to the need to go to the toilet. Many people report feeling that they constantly need to wee, which negatively impacts their life.
People who leak urine in addition to their OAB is experiencing incontinence. Stress urinary incontinence (SUI) occurs when someone leaks urine when laughing, sneezing, or straining from physical exercise. SUI is a different condition than OAB, you can have both issues concurrently. We sell a wide range of incontinence pads for the elderly which can be used to help manage symptoms associated with this condition.
Learn more about Stress incontinence
Overactive bladders - what you need to know
- What Is An Overactive Bladder?
- Overactive Bladder Syndrome Symptoms
- When Should You See A Doctor For OAB?
- Key Statistics
- How Is An Overactive Bladder Diagnosed?
- Ask You To Keep A Bladder Diary
- Perform a Physical Exam and Conduct Basic Tests
- How The Urinary Tracts Works, And What Causes An Overactive Bladder
- Complications
- Risk Factors For An Overactive Bladder
- Prevention
- Treatments
- Who Treats Overactive Bladders?
- Tips To Help You With Your Doctor’s Visit
- Questions to Ask your Doctor about OAB
- Sources list
Overactive Bladder Syndrome Symptoms
People experiencing the problems associated with an OAB may experience some or all of the following symptoms2:
- Urinating more frequently than is normal (8 or more times in a 24 hour period)
- Urge incontinence (involuntary urination that follows the urgent need to urinate, without making it to the toilet
- Waking up in the night two or more times to urinate (nocturia)
- Constant worrying and fretting about needing to urinate, and the fear of not making it to the toilet in time
- ‘Wetting the bed’ (Nocturnal Enuresis)
- Leaking urine during sexual activity (Coital Incontinence)
These symptoms will interrupt an individual’s daily life, and can cause mental and physical stress over a prolonged period of time.
When Should You See A Doctor For OAB?
While you might think that an OAB is ‘just a part of getting older,’ these bladder symptoms are not a normal part of the aging process. It is common amongst older adults, but it does not have to be. If you have an OAB, you are likely feeling stressed, embarrassed, and frustrated.
While OAB can happen to anyone, the problem tends to increase with age. As many women believe that this is a natural consequence of childbirth, they don’t seek help, assuming that there are no solutions. Both men and women are reluctant to speak with their GP out of embarrassment.
You might feel nervous about speaking with your doctor about this issue, but it is well worth doing so. They can examine you to ensure that it isn’t a symptom of a more serious illness, and help you with solutions.

Key Statistics
Men, women, and children of all ages experience overactive bladder (OAB) symptoms, but most sufferers are older women. A large NHS study conducted in the UK found that roughly 1 in 6 adults experienced OAB symptoms3 to some degree, and with varying levels of severity. Approximately one in three of these also experience urge incontinence.
It has been estimated that up to 30% of men in the UK and 40% of women are struggling with OAB symptoms. The exact number is unknown, due to the fact that many people do not seek help or treatment for the problem.
How Is An Overactive Bladder Diagnosed?
If you suspect you might have an overactive bladder (OAB), you should first make an appointment with your GP. They will then ask you a series of questions about your medical history and family background. Following this, they will give you a physical examination, and ask you to provide a urine sample.
Your urine sample will be tested for infection or other problems that could explain your OAB symptoms. If none are present, you might be referred to a specialist for further assessment.
Here are some of the things that your doctor might do to diagnose OAB:
Ask You To Keep A Bladder Diary
Your doctor might ask you to keep a bladder diary so that they can glean useful information. They might ask you to record the following information:
- everything you drank, including when and how much
- every time you urinate, and how long urination takes
- the urgency that you felt before each visit to the toilet
- if you experienced any incontinence
Perform a Physical Exam and Conduct Basic Tests
Your GP might perform a physical exam and take tests after taking your medical history. These exams and tests can include4:
- A pelvic or prostate examination
If you have a female pelvic examination, your doctor will assess you for any vaginal abnormalities, and check the strength of your pelvic floor muscles. A male prostate examination will check for an enlarged prostate, something that could cause OAB symptoms.
- Neurological examination
Your GP may want to assess your sensory responses and reflexes to determine if a neurological issue might be causing your OAB symptoms.
- Cough stress test
A cough stress test might be conducted to rule out the possibility of stress incontinence. You will be asked to drink liquids, relax, and then cough. This will assess if physical stress is causing urinary incontinence.
- Urinalysis
In almost all cases, you will be asked to provide a urine sample. This will be sent to the lab to be checked for abnormalities, including high levels of blood bacteria, or glucose. If you have too much bacteria in your urine, you may have a urinary tract infection (UTI). Too much glucose can be a sign of diabetes.
- Urodynamic tests
Urodynamic tests are designed to measure your bladder’s ability to empty fully and completely, and if your bladder is contracting involuntarily. This involves a catheter being inserted into your bladder through your urethra in order to measure how much urine is left in your bladder after urination, and your bladder’s capacity. Continence Nurse Specialists can carry out a less invasive test using a bladder scanner, which measures the volume of residual urine that remains post voiding.
- Uroflowmetry
During Uflowmetry, you urinate into a uroflowmeter machine, which measures the speed and volume of your urination.
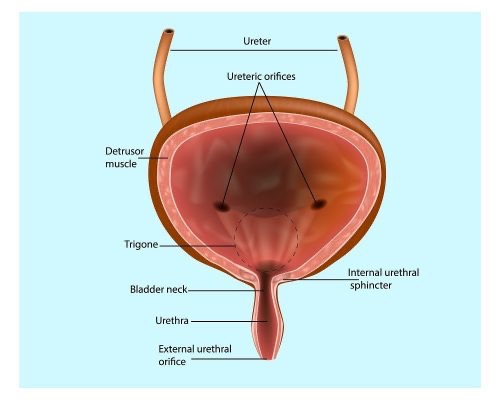
How The Urinary Tracts Works, And What Causes An Overactive Bladder
Your urinary tract5 is one of the vital systems in your body, important because it removes the liquid waste from your body. The urinary tract includes:
Kidneys: 2 organs that filter the waste from your blood, and help to produce urine from the
Ureters: 2 thin tubes that transport urine from your kidneys to your bladder.
Bladder: the muscular sac that can expand to store your urine until it is time for urination.
Urethra: the tube that carries the urine from your bladder out of your body. Your urethra has a sphincter muscle that helps to prevent urine from escaping.
In a healthy person, the brain sends a signal to the bladder when it is full of urine. The bladder muscles squeeze together, and urine is forced out of the urethra. The urethral sphincter opens, and urine flows.
With OAB, your brain sends the signal too late, and so the need to urinate feels urgent. The nerve signals don’t work correctly, causing you to feel like you ‘have to go’ urgently, even when your bladder is empty.
Complications – How Can OAB Affect Your Life?
If you have OAB, you might experience all kinds of negative mental and physical symptoms. These include:
- Withdrawing from social or work activities
- Poor quality of sleep, and constantly feeling tired
- Depression
- Embarrassment over frequent trips to the toilet
- Soiling or staining your clothing and bedding
- Anxiety and panic
- Falls and hip fractures in older people as they rush to get to the toilet

Risk Factors For An Overactive Bladder
Some of the most common risk factors for OAB include:
- Medication side effects
- Hormonal changes
- UTI (urinary tract infections)
- Neurological disorders
- Pelvic spasms or muscle weakness
- Multiple Sclerosis
- Stroke
- Alzheimer’s Disease and other cognitive decline
As you age, you are more at risk for OAB. For people with cognitive decline, incontinence resulting from OAB can be managed with timed and prompted urination, fluid schedules, and incontinence supplies.
Prevention
If you want to prevent the symptoms of OAB before they occur, follow these tips for prevention:
● Reduce to and maintain a healthy weight for your age and height
● Do regular physical exercise. Learn how Incontinence and sport work well together
● Don’t smoke
● Limit the amount of alcohol that you drink
● Limit your consumption of caffeinated and acidic drinks and other drinks that can cause irritation in the bladder.
● Manage your diabetes
● Check regularly your mental health professional
● Strengthen your pelvic floor muscles by doing pelvic floor exercises

Treatments For Overactive Bladder
If your GP or specialist diagnoses you with OAB, they may recommend one or more of the following treatment plans.
- Avoid caffeine, alcohol, chocolate, and citrus fruit drinks, as these can all stimulate the bladder
- Increase the amount of water you drink
- Practice double voiding – void your bladder as usual, wait a few seconds, and then try again
- Practice delayed urination – delay the timings between your instances of urination
- Practice pelvic floor exercises to strengthen and relax your bladder muscles
- Time your urination, and keep to a strict urination schedule whether you feel you have to go or not
- Prescribed medications (for example: Anti-muscarenics and Beta-3 agonists) that can help your bladder to relax and stop contracting when it is not full
- Bladder Botox Treatment6 – small injections of Botox can gently paralyse the muscles in your bladder, and last for 6 -12 months
- Nerve Stimulation7– Percutaneous tibial nerve stimulation (PTNS) and Sacral neuromodulation (SNS) have both been shown to help with the symptoms of OAB
- Bladder Reconstruction/Urinary Diversion Surgery – These surgeries re-route the flow of urine, and are only used in the rarest and most severe cases.
Who Treats Overactive Bladders?
On your journey to diagnose and treat OAB, you might see some or all of the following medical practitioners.
- Primary Care Practitioners – your GP can diagnose and treat OAB.
- Urologists – surgeons who specialise in the urinary tract.
- Gynaecologists – doctors who focus on women’s health, including the urinary tract.
- Nurse Practitioners (NP) – highly trained nurses who can diagnose and treat OAB.
- Physician Assistants (PA) – professionals who can diagnose and treat OAB under the oversight of a doctor.
- Geriatricians – doctors who specialise in treating older patients.
- Bladder and Bowel Service – nurses who are specialised in bladder and bowel management
- Physical Therapists – licensed health professionals, some of whom provide pelvic floor physical therapy.

Tips To Help You With Your Doctor’s Visit
It can be easy to become overwhelmed when you get into the examination room with your GP or a specialist, forgetting all of the questions you had planned to ask. As you prepare for your doctor’s appointment to deal with your OAB, here are some tips that can help you get the treatment that you need. Being prepared not only helps you, it also helps the health care provider.
- Bring the following:
- A list of your medical history, including all past and present illnesses, operations / procedures
- A list of all of the medications you are currently taking, including vitamins, herbs, prescription drugs, and over-the-counter medicines
- A paper and pen to take notes
- Ask a friend or family member to come along – Bringing a trusted relative or friend with you can help you to remember your questions, and help remind you of the things that the doctor says.
- Bring up your OAB symptoms – Your doctor might not mention your OAB symptoms, so be sure to mention them at the beginning of your appointment. Do not be embarrassed – they have heard all of these things before.
- Don’t be afraid to ask questions – You should feel free and able to ask all of the questions on your mind. if you can’t think of any specific questions of your own, read ahead for some examples you can use.
- Ask for samples of incontinence products. It is important to choose the correct one, to feel comfortable and safe.
Incontinence Product Finder
Selecting the right products is key in ensuring security and discretion. If you’re not quite sure what you need, try our product finder. It’ll ask you a few questions about your needs and then provide a list of recommended products that may help you.
Find Product Incontinence Product FinderQuestions to Ask your Doctor about OAB
- Do I have OAB, or are my symptoms caused by something else?
- What tests will I undergo?
- Did something specific cause my OAB?
- What can I do to prevent or ease my OAB symptoms?
- If I don’t treat my OAB, what will happen?
- What lifestyle changes can I make?
- What exercises can I do?
- Should I start seeing a physical therapist?
- Do you have suggestions for treatments that could help my OAB?
- When will I start to feel better?
- Are there side effects from these treatments?
- Will I need to seek these treatments forever?
Summary
It is important to know that help and support is available if you are suffering from symptoms of an overactive bladder – it’s time to take your life back from OAB. You will know how it feels to feel good again as you start to make progress on your journey to a healthier bladder. Remember, there is hope and help out there, with the right advice and treatment.
Sources
- The Independent (2018). ‘It was mortifying’ – The embarrassing issue suffered by hundreds of thousands of Irish women every day. [online] Available at: http://independent.ie/life/health-wellbeing/it-was-mortifying-the-embarrassing-issue-suffered-by-hundreds-of-thousands-of-irish-women-every-day-37114309.html [Accessed 23 Oct. 2019].
- The Independent (2018). ‘It was mortifying’ – The embarrassing issue suffered by hundreds of thousands of Irish women every day. [online] Available at: http://independent.ie/life/health-wellbeing/it-was-mortifying-the-embarrassing-issue-suffered-by-hundreds-of-thousands-of-irish-women-every-day-37114309.html [Accessed 23 Oct. 2019].
- Urologyhealth.org. (2019). Overactive Bladder (OAB) – Urology Care Foundation. [online] Available at: https://www.urologyhealth.org/urologic-conditions/overactive-bladder-(oab) [Accessed 23 Oct. 2019].
- Mft.nhs.uk. (2019). [online] Available at: https://mft.nhs.uk/app/uploads/sites/4/2018/04/Overactive-bladder-August-2017.pdf [Accessed 23 Oct. 2019].
- Healthline. (2019). Overactive Bladder Diagnosis: What Tests to Expect. [online] Available at: https://www.healthline.com/health/overactive-bladder-diagnosis [Accessed 23 Oct. 2019].
- Urologyhealth.org. (2019). Overactive Bladder (OAB) – Urology Care Foundation. [online] Available at: https://www.urologyhealth.org/urologic-conditions/overactive-bladder-(oab) [Accessed 23 Oct. 2019]
- mkuh.nhs.uk (2022). Botox Injections for the treatment of an overactive bladder – NHS – [online] Available at:https://www.mkuh.nhs.uk/patient-information-leaflet/botox-injections-for-the-treatment-of-an-overactive-bladder-2
- www.nice.org.uk. Percutaneous posterior tibial nerve stimulation for overactive bladder syndrome- Nation Institute for Health and Care Excellence – NICE. [online] Available at: https://www.nice.org.uk/Guidance/IPG362 [Accessed 13.06.2022]

MoliCare Pad 4 Drops
<h2>Handy MoliCare Pad 4 Drops to Carry on the Go</h2> <p>Our MoliCare® Pad 4 Drops are an essential product for those experiencing slight incontinence, allowing you to regain control and live your busy and active life without the interference of bladder weakness. Designed for both men and women, this pad for men and women offers exceptional dryness and protection, ensuring your comfort and confidence.</p> <h2>‘Barely There’ Reassurance and Reliability</h2> <p>The MoliCare® Pad 4 Drops are slimline, discreet, and adjusted to fit your body seamlessly. It fixes securely inside your underwear, providing a ‘barely there’ comfort feel. With its soft and skin-kind fabric, along with a wide adhesive fixing strip on the backsheet, you can go about your day with the assurance of being protected against leakages.</p> <p>The absorbent core effectively prevents your skin from becoming too moist, while the elastic anti-leak edging adds an extra layer of security and peace of mind. Say goodbye to any worries about odours, as the MoliCare® Pad 4 Drops also neutralises odours to keep you fresh and confident throughout the day. Don't let incontinence hold you back from living life to the fullest.</p> <p>Ordering your MoliCare® Pad 4 Drops is hassle-free, as we offer fast and discreet delivery direct to your door. With our price match promise, you can trust that you're getting the best value for your money. Plus, enjoy free delivery on all orders over £40.</p> <p>If you need assistance in finding the perfect incontinence product for your needs, our friendly customer care team is here to help. Don't hesitate to reach out to us at 0800 028 9470. Take control of your life with the reliable protection and comfort of the MoliCare® Pad, alongside other <a href="https://www.hartmanndirect.co.uk/incontinence-products/incontinence-pads" style="color:#0563c1; text-decoration:underline">incontinence pads</a>.</p> <p> </p>
MoliCare Pads for Day
<h3>Incontinence pads for protection during the day </h3> <p>Even slight bladder weakness can be a burden in everyday life. There is a simple and affordable solution for this: MoliCare® Pad Day delivers discreet, reliable protection that helps you manage life’s daily challenges. </p> <p>The highly absorbent core inside the incontinence pads quickly locks away urine to ensure a pleasantly dry feeling on the skin. At the same time, it neutralises unpleasant odours. </p> <p>MoliCare® Pad Day are designed for discreet protection during the day. You can recognise the daytime incontinence product by the sun symbol on the packaging. They complement MoliCare® Pad Night incontinence pads which provide reliable protection at night. </p> <h3>Who is MoliCare® Pad Day suitable for? </h3> <p>MoliCare® Pad Day incontinence pads are suitable for people with mild bladder weakness. They leak anywhere from a few drops to 100 ml of urine between visits to the toilet. </p> <p>Incontinence pads are suitable for active women and men users whose mobility is not restricted. They can go to the toilet independently and without assistance. </p> <h3>Cheap incontinence products: comfortable, discreet protection </h3> <p>The incontinence pads have a highly absorbent core and odour control to keep you feeling fresh and comfortable. Thin and flexible, MoliCare® Pad Day are designed to be discreet, invisible under your clothing. Thanks to the wide adhesive strip, they remain securely in place even during sport. The incontinence pads are made from soft, breathable material so you feel comfortable all day. </p> <p>You usually need no more than two MoliCare® Pad Day incontinence pads during the day and one MoliCare® Pad Night incontinence pad for undisturbed sleep. This gives you a low cost yet high-quality round-the-clock supply of incontinence pads from HARTMANN. </p> <h3>We are HARTMANN </h3> <p>MoliCare® is HARTMANN’s extensive range of continence care. For over 40 years, we have been developing effective, reliable products that help people manage the challenges of living with incontinence. Our aim is to provide the right solution for every need. </p>
MoliCare® Premium Lady Pad 3 Drops
<h2>Lightweight Incontinence Solutions</h2> <p>The MoliCare® Premium Lady Pad 3 Drops is the perfect solution for women who are looking for a slim, discreet and comfortable way to manage slight bladder incontinence situations. The pad is small and lightweight, so it's easy to carry with you on the go. And the odour neutralisers help to keep you feeling fresh and confident all day long.</p> <p>With a fast and reliable delivery, you can apply your MoliCare® Premium Lady Pad 3 drops in next to no time. With their compact appearance, they are easy to apply and are barely noticeable when fitted under your underwear. For extra skin-friendly protection, we equip these products with Aloe Vera to maintain a healthy skin, as well as absorbent and secure technology. It is truly one-size fits all with this range!</p> <h2>Maintain peace of mind</h2> <p>These lady pads contain 14 pieces per bag, are set at an affordable pricing, and will prevent leakages, maintaining peace of mind in all social situations.</p> <p>If you require additional information, do not hesitate to get in touch with our reliable customer service team, who are ready on hand to answer your questions. If you're looking for a reliable pad that will help you stay dry and comfortable, the MoliCare® Premium Lady Pad 3 Drops is a great option. Order yours today!</p>
